
The MDP-based adhesive functional monomer found in various Ivoclar products has been specially formulated to ensure high bond strengths to various substrates.
MDP consists of a long-chain methacrylate with a phosphoric acid group.
The phosphoric acid group enables a stable chemical bond to zirconium oxide and base metal alloys. Consequently, using an additional bonding agent or primer is not required for permanent bonding to these restoration substrates.
In addition, phosphoric acid reacts with the calcium ions of the dental hard tissues and, in the process, produces a bond with the tooth structure. The need for a separate adhesive is eliminated.
Which Ivoclar products contain 10MDP?
1. Tetric N-Bond Universal – The Universal adhesive for bonding direct and indirect restorations. The acidic monomer MDP bonds to the calcium within the hydroxy apatite to form insoluble calcium salts, facilitating mechanical blockage and sealing in the dentin tubules. This helps prevent the movement of fluid in the dentin as well as post-operative sensitivity associated with that movement.

2. Monobond N – The universal primer for conditioning of all indirect restorations. The acid monomer MDP improves bond strength to zirconia and metal surfaces. The MDP bonds to zirconia on its free phosphate group and to resin cements on its methacrylate end.
Monobond N is distinguished by an innovative combination of three different functional adhesive monomers: phosphoric acid methacrylate, silane methacrylate and sulfide methacrylate. This combination enables the universal primer to bond to zirconia, glass-ceramics and metal alloys.

3. Multilink Speed - A clinically proven self-adhesive resin cement with MDP within its formulation for the permanent seating of high-strength restorations made of zirconia and metal, both on natural teeth and implant abutments. Given its self-curing, self-adhesive properties, Multilink Speed offers peace of mind and security, especially when cementing opaque restorations.

Zirconia (zirconium oxide)-based ceramics have become a very popular type of all-ceramic restorations. Zirconia-based ceramics have a high strength and, therefore, restorations can be cemented with traditional cements or bonded with resin cements.
Zirconia crowns and bridges with adequate thickness, good retention and fit, do not need bonding (do not rely on high bond strengths) and can be cemented with conventional cements.
If greater retention to tooth structure with minimal marginal leakage is required, bonded cementation with resin cements is recommended. Adhesion to tooth structure and to the ceramic restoration combines good marginal sealing and strengthening of the tooth-restoration complex to minimize marginal leakage and tooth fractures.
Conventional cementation with glass-ionomer cement (GIC), resin-modified glass-ionomer cement (RMGIC) or self-adhesive resin cement - If your cement does not contain the MDP (as in the case with GICs, RMGIs, some self-adhesive resin cements and all adhesive resin cements), a MDP primer needs to be applied to the fitting surface of the restoration.
If your cement already contains MDP within its formulation (as in the case with Multilink Speed), a MDP primer is not required on the fitting surface of your restoration.
Self-adhesive resin cements are the best choice for zirconia-based ceramic restorations, when the restoration does not require the highest retention.
Self-adhesive resin cements are less technique sensitive than bonding with adhesive resin cements and offer more retention and better marginal sealing of tooth structure than the traditional glass ionomer cements. No separate bonding agent is necessary, reducing much time and effort, and cleanup is easy with self-adhesive resin cements.
When more retention is needed due to a short clinical crown or an over tapered preparation, adhesive resin cements, may be used to bond the restoration. Adhesive resin cements do not contain MDP within its formulation and therefore a primer to the restoration surface and a bonding agent is to be applied to the tooth surface.
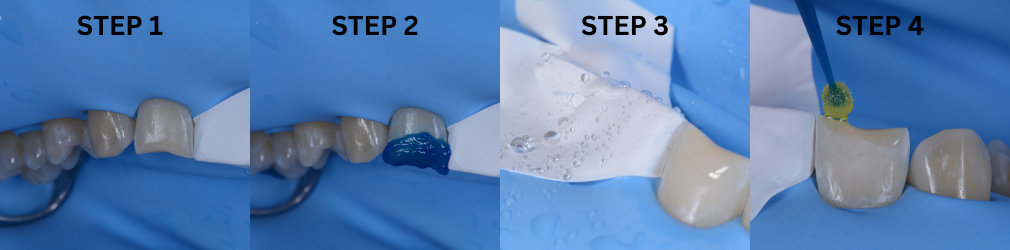
Zirconia cementation with Multilink Speed – your self-adhesive resin cement:
Air-particle abrasion (sandblasting) of the zirconia restoration before cementation - 30-60ų alumina particles for 5 seconds. This is done by your dental laboratory after fabrication of the restoration.
1. CLEANING: During try-in the restoration becomes contaminated with phospholipids, saliva and blood. The intaglio of the crown therefor has to be cleaned with a special ceramic cleaner after try-in. Ivoclean is the universal extra-oral cleaning agent for the decontamination of the fitting surfaces of restorations after try-in.
2. APPLY CEMENT: Apply cement into restoration and seat on tooth. No zirconia primer is required when using Multilink Speed, as it already contains the acidic monomer MDP within the cement formulation. No bonding agent is required on the tooth surface as the acidic monomer MDP within the cement formulation bonds to the calcium within the hydroxy apatite to form insoluble calcium salts facilitating mechanical blockage and sealing in the dentin tubules.
Zirconia cementation with Variolink Esthetic DC – your dual curing esthetic adhesive resin cement:
Air-particle abrasion (sandblasting) of the zirconia restoration before cementation - 30-60ų alumina particles for 5 seconds. This is done by your dental laboratory after fabrication of the restoration.
1. CLEANING: During try-in the restoration becomes contaminated with phospholipids, saliva and blood. The intaglio of the crown therefor has to be cleaned with a special ceramic cleaner after try-in. Ivoclean the universal extra-oral cleaning paste for the decontamination of the fitting surfaces of restorations after try-in.
2. CERAMIC PRIMER: The adhesive resin cement Variolink Esthetic does not contain the acid monomer MDP within its formulation and therefor a ceramic primer containing MDP needs to be applied to the fitting surface of your restoration. Monobond N the universal ceramic primer with MDP is used.
3. TOOTH SURFACE: All adhesive resin cements require the tooth surface to be bonded with a separate bonding agent. Tetric N-Bond Universal is used on the tooth surface, dispersed with air and cured.
4. APPLY CEMENT: Apply Variolink Esthetic DC resin cement into restoration and seat on tooth.

Dr. Giuseppe Chiodera, an honorary member of Style Italiano, loves developing new treatment techniques that simplify diagnostic and restorative procedures.
Lucida Paste a sub-micron hybrid water-soluble patented polishing compound for extreme gloss in combination with the felts.
For more product information click here.


Clinical Management of Deep Subgingival Margin Elevation in Posterior Teeth with Structural Compromise.
The understanding of restorative dentistry today demands not only considering the preservation of remaining tissues but also respecting the biomechanics governing the dental structures, having as main objectives the preservation of pulpal health and strengthening fragile and more affected teeth, providing a clinical treatment with the longest possible lifespan.
Within routine clinical practice, restorative concepts and techniques aim to bioemulate lost tissues in terms of structure and function. Precisely one of the most demanded techniques today for our indirect restorative procedures is the relocation of cervical margins or deep margin elevation. This clinical approach was first described in 1998 by Dietschi and Spreafico, who defined it as "a technique indicated in cases with slightly subgingival margins, where it is possible to relocate the cervical area of a preparation more coronally by applying appropriate increments of composite resin on the existing margin. This procedure should be developed under absolute isolation with a rubber dam, followed by the placement of a metal matrix band" (1). Since the introduction of this new concept, other authors and publications have emerged, emulating the technique, and applying it to various scenarios in restorative dentistry. In terms of posterior indirect partial restorations, elevating the cervical margin of a preparation above the gingival margin provides advantages for impression taking and subsequent isolation during the cementation process. However, fundamental requirements must be taken into consideration in order to ensure a correct adhesive procedure: complete isolation of the cervical margin of the preparation and placement of a matrix band that achieves perfect sealing of the cervical area. Otherwise, the technique is contraindicated.
Once the technique is performed, a bitewing radiograph should be taken to evaluate the adaptation of the composite resin in the gingival area, checking for gaps or over-contours before proceeding with the final impression (2).
In terms of clinical elements to consider for correct clinical performance, a curved matrix is recommended to ensure not only perfect sealing in the gingival area but also the formation of a correct emergence profile. In this situation, the use of ReelMatrix™ margin elevation bands from Garrison (Fig. 1) is recommended. Due to their thickness, contour, and height, these bands achieve anatomical margin elevation in most cases. Like other bands designed by the same company, they have two different surfaces: one coated with Teflon to improve handling of the restorative material and another with a rigid metallic surface. This band, which was specially designed for this technique, should be attached using a tensioning instrument (Fig. 2) which places this band on the cervical margin of the preparation with efficiency and precision.
Clinical Case
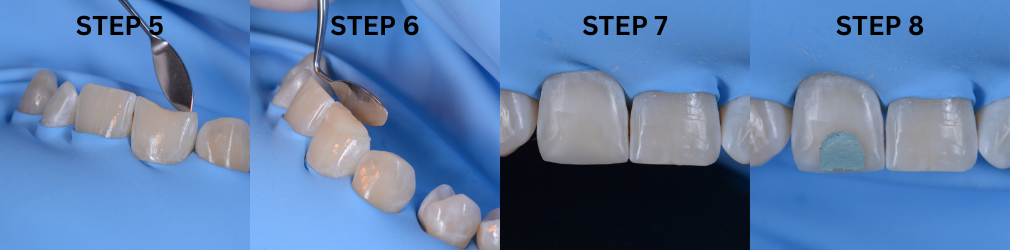
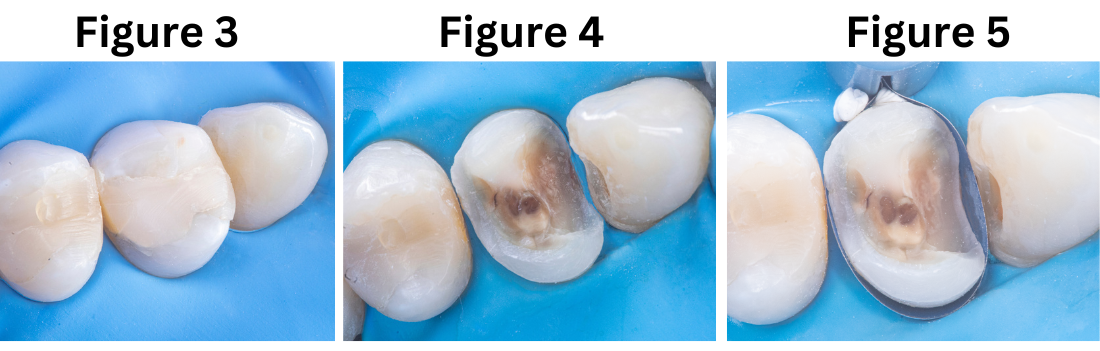
A 20-year-old female patient visits the dental clinic due to moderate pain and expresses a desire to replace an old restoration. Upon clinical examination, a composite resin restoration partially covering the occlusal surface of tooth 2.4 is observed, showing marginal gaps, secondary caries, and deficient anatomy (Fig. 3). Based on the specific structural diagnosis, an indirect composite resin restoration on a stress-controlled biobase was indicated. This will maximize adhesive strength through a rigorous biomimetic restorative protocol associated with deep margin elevation in the mesial proximal box without the need for prior surgical intervention.
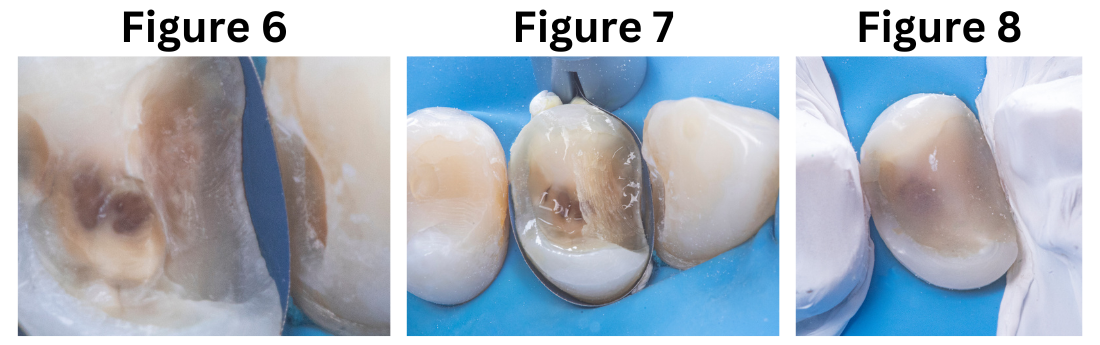
The procedure described above was performed in two phases. The first phase focused on primarily replacing the dentin, for which the old restoration was completely removed (Fig. 4). Subsequently, the tensor-band complex was placed to elevate the cervical margin using the ReelMatrix™ Deep margin Elevation system (Fig. 5). The image shows the band's adaptation to the tooth, achieving a perfect marginal seal (Fig. 6). Immediately after, the adhesive phase was complete, followed by the application of a hydrophobic layer of Flow and finally a 3mm strip of polyethylene fiber to ensure adhesion, along with a thin layer of (Fig. 7). Subsequently, layers of composite resin, not exceeding 1mm in thickness, were applied to achieve progressive buildup. Once the biobase was established, a minimal biological preparation was performed using diamond burs, and a definitive impression was taken for the fabrication of the indirect restoration (Fig. 8).
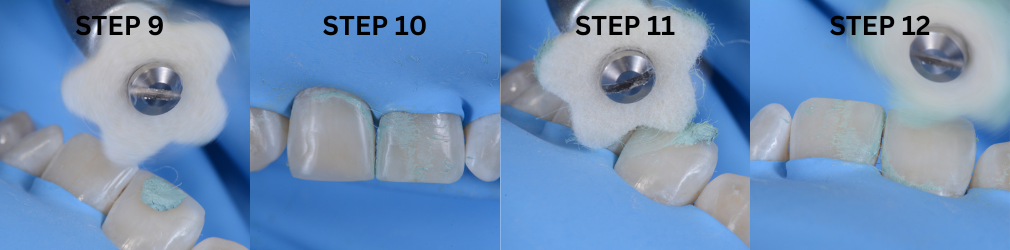
In the second phase, under absolute isolation, the indirect restoration was connected to the previously constructed biobase using an adhesive bonding agent, to ensure high mechanical properties and favorable aesthetics. Excess material was carefully removed, mainly in proximal areas, and after curing, the rubber dam was removed for the final view of the restoration, evaluating harmony with the periodontal tissue and occlusion (Fig. 9+10).


References
Bio for Dr. Patricio Gutiérrez:
Dr. Gutierrez is a graduate of the dental school of the Pedro de Valdivia University, in Santiago, Chile.
He has carried out his entire career in the private sector, in different private clinics located in Santiago.
Since he got his degree, Dr. Gutierrez has trained and practiced restorative and aesthetic dentistry, this being his area of interest. In 2016, he participated in the aesthetics diploma in adhesive oral rehabilitation at the dental school of the University of Los Andes, in Santiago. After that, he held teaching positions at universities and institutes contributing to numerous publications and clinical cases. This vocation led him to obtain a Magister in Higher Education at the Andres Bello University.
Currently, Dr. Gutierrez is studying towards a Diploma in Restorative Dentistry Biomimicry at Diego Portales University, also in the same city Santiago.
Over the past couple of years, Dr Gutierrez, has dedicated himself exclusively to this area, becoming an "opinion leader" of different commercial dental brands that are established in Chile.
View product on IvodentOnline here.

How long have you been using e.max and what is your experience with it?
I have used e.max extensively over the past 12years – as long as I have worked in South Africa – and was one of the first people to use it. I’ve done almost six thousand restorations using e.max and haven’t found any other material that matches up to it. Its longevity and aesthetics is impressive.
What are your key reasons for choosing to use e.max
In the past dentists have had to compromise on materials that look good but don’t last very long. e.max restorations have both beauty and long life. It also allows us to apply minimally invasive protocols as a more conservative approach to restorations. I can restore the teeth without having to destroy them first. It fits our need in every way and is an absolute win-win option. IVOCLAR has managed to create a material that adapts to each patient – colour, aesthetics… etc. It fits seamlessly into where dentistry is going – from analogue to digital – the adaptation has been done – and Ivoclar is ahead of the game.
Longevity and aesthetics are the key cornerstones in dentistry – we always had to compromise…. Now we have the best of both worlds with e.max.
In the 12 years I have been working with e.max I have had the time to see and evaluate the cases…..and I am even more enthusiastic now I can see the longevity!!
I love its versatility – I can do the front and back of mouth and implants.
Ivoclar has had the opportunity to develop something in a way that fits our needs in a big way – it is an outstanding option.
The materials are designed to fit every case – no longer is it necessary to compromise on lifespan in favour of quality.
Because no two cases are the same, Ivoclar has managed to create a material that adapts to each patient – colour, aesthetics… etc.
Some dentists do resist changes but I have adapted, from single teeth to full mouth rehabilitations. I run an aesthetic and restorative practice. It fits into where dentistry is going – from analogue to digital – the adaptation has been done – and Ivoclar is ahead of the game…
The versatility of materials is exciting, I can use an ingot hand-made (wax and press) or milled in a block, design CAD and CAM and mill!
Very few materials have long term research to back up long-term claims – I have confidence due to the success I have achieved over the years, supported by the clinical research.
I love the predictability of the material – successful delivery, treatment and longevity benefits both me and the patient financially and brings credibility and satisfaction.
Dr Bowes is a Fellow of the International Congress of Oral Implantologists; practised in London for 23years and in 2010 founded the South African Academy of Aesthetic Dentistry. He runs a private practice in Cape Town, focussed on Aesthetic and Complex Restorative Dentistry. He is a member and registered speaker for the ITI – International Team for Implantology. As Founder and past president of the South African Academy of Aesthetic Dentistry, he has pioneered the development of Digital Smile Design in South Africa, enabling dentists to develop a smile which fits both aesthetic and functional needs for each individual. As a DSD World Master and Instructor, he lectures and teaches both in Southern Africa and internationally. He is passionate about minimally invasive treatment and has introduced IAS – Intelligent Aligner Systems to South Africa, running courses to teach fellow dentists. Mark has recently been invited to be a silver member of the prestigious group Styleitaliano and an honorary global ambassador for @slowdentistry. He is an ambassador of the Humble Smile Foundation – a global group of dental and development professionals who passionately promote oral health and prevent oral disease as an integral part of children’s well-being.
Click here for more e.max product info and IVOdeals.

I have been using e.max in my practice for almost 15years and I can say in all confidence that it surpasses any other material I have ever used before. It’s more superior as it’s the most stable and versatile material for the job at hand. I can go home and sleep well at night knowing I do not have to worry about the work done, confident that no problems will be experienced.
I use it mainly for crown and bridge work, full rehabilitation cases and have more recently moved into doing a large amount of inlays and onlays, implant based crowns … pretty much everything actually - there really is nothing we can’t use it for!
More and more we get patients who come in and demand “the real e.max material”. So much so that we use e.max stickers to put on their invoices and cards to prove to them we have used it. I find patients nowadays are well prepared and educated and come to us having done their homework and well aware of all the options available to them. They do not want Zirconia at all. We last saw this with daVinci Porcelain; patients knew about it and asked for it. Now they ask for e.max.
The strength angle is overrated; there are stronger materials out there, but for me, why I find it superior for the job is that it’s an all-rounder – combining strength, versatility, aesthetics and bondability. When you learn how to properly process and bond it, what more do you want!? And of course it’s proven, not just in my hands, but in many, many published reports.
I conduct a lot of CADCAM training courses, and in fact am doing an anterior course this week, and I always tell doctors on my courses how essential it is to have e.max as a staple in their practice and we teach and show them how to manage and process it and tell them that they can advocate it with 100% confidence. I tell them “e.max is the GO TO block!”
Dr Vikash Naidoo graduated from the University of Witwatersrand in 2001, and entered private practice soon after qualifying. Very early on in his career he showed a flair for cosmetic dentistry, and soon thereafter incorporated the art of computerized cosmetic dentistry into his practice. His passion for the computerized cosmetic world of dentistry is such that he has become an international certified CEREC trainer, and derives great satisfaction in training dentists who are new to the CEREC community.
Being invested in computerized dentistry has allowed Vikash to travel the globe, ensuring that he is at the cutting edge of the latest developments in this digital area. Technology has rapidly progressed over the past decade, making dentistry easier, precise, highly efficient and less traumatic, a doctrine Vikash embraces completely. Vikash realised that cosmetically enhancing a patient’s smile, is in most cases only one part of the equation, resulting in him becoming an accredited Dermal filler practitioner, allowing a holistic approach to facial aesthetics. He also has completed a number of post graduate surgical implant courses through the much respected Implant Academy, placing him in a perfect position to be able to complete an excellent standard of comprehensive care. Dr Vikash Naidoo is an Executive member of the South African Academy of Cosmetic Dentistry (SAACD), and participating member of the International Society of Clinical Dentistry (ISCD), South African Dental Association (SADA) and Health Professions Council of South Africa (HPCSA).
Click here for more e.max product info and IVOdeals.

How long have you been using e.max?
I have worked with bonding ceramics for 34yrs; prior to e.max I used EMpress 1 and EMpress 2.
e.max revolutionised the dental industry, mainly due to its strength and versatility. I have been using it since its arrival on the South African scene, and it has added exceptional value both to my practice and to dentistry as a whole!
It seems to require 30yrs for a paradigm shift to occur in dentistry and this has now happened, with bonded ceramics being adopted as the treatment of choice in indirect restorations. It’s very exciting - especially with e.max!
What do you like most about using the product?
I like the fact that you can use e-max equally well for veneers, inlays, onlays as well as full crowns. So it’s one product for very many different applications. Being able to use the same ceramic throughout allows for conformity of colour and texture which maximises aesthetic outcomes. With e.max offering copings in five different translucency levels each with multiple shades, this allows even more versatility – catering for all needs, no matter the colour of the underlying tooth structure. It’s just like a box of chocolates – sometimes I feel like a chef…. you can pick and choose and create the proper recipe for a particular situation for ultimate perfection!
Also it gives you the option of going monolithic for strength, or a layered technique can be utilized for better aesthetics – incredible flexibility in aesthetics…. Just brilliant! Bonded ceramics is definitely my preferred choice as opposed to conventional cemented crowns.
What I really like about e.max and bonded ceramics is that it is very strong even in thin layers, ideal for veneers and table top overlays. It’s minimally invasive, as opposed to the traditional methods. With patients getting older and living longer we need to do more minimally invasive treatments and also treatments that help teeth last much longer than before - they need to last a lifetime! The e.max durability is the perfect solution.
Furthermore, depending on the application and design it can be luted with fully adhesive techniques, self-adhesive techniques or conventional cementation techniques. Due to these flexible cementation options we are able to offer reliability and ease of use for the appropriate situation.
And the fact that it is available in the analogue press technique or for the digital CAD Cam applications, is great.
Another positive with ceramic restoration is that it’s EASY to use; it can be prepped with traditional hydrofluoric acid plus silane or the new impressive and convenient, “monobond etch and prime” solution.
It’s EASY to adjust and polish, even intra-orally after cementation, should it be required.
What would you like to share with other dentists about using e.max?
Ultimately what sells it for me after all my years of using e.max in my practice, is the feeling I get when patients who had major restorations done previously, come in for check-ups years down the line and I look in their mouths only to see a perfect dentition with nothing needing to be done. e.max is so durable that it’s almost unnecessary to have wasted their time for a follow up examination, as I can almost predict even before examining them, that everything will be in great shape. Nevertheless it always gives me a kick to be able to give them a clear bill of health…. to say nothing needs to be done today”….Your teeth are perfect! Any problems are usually very minor in the form of a small chip or something similar, which can easily be repaired and polished intraorally to continue the durability and longevity!
Essentially e.max equates to COST EFFECTIVE dentistry…. The return on investment is huge and long term – very few, problems if any occur down the line – actually it is not only FINANCIALLY cost effective but most importantly is BIOLOGICALLY cost effective – as by using minimally invasive treatment options and keeping the mouth in tip top condition, it maintains overall body health!
Dr Effting graduated at the University of Witwatersrand as the Best All Round Student and is senior dentist and clinical director of Hout Bay Dental Studio in the Western Cape. With nearly 40yrs experience, he has a particular interest in mercury-free, minimally invasive dentistry with wide experience in implantology and in treating patients in a holistic manner. He is a founding member and President of the South African Academy of Aesthetic Dentistry and Fellow of the International Team of Implantology. In his spare time he is a keen sportsman with a particular love of cycling.
Click here for more e.max product info and IVOdeals.